Statistically, male factor infertility is observed in almost 40–50% of the total infertility cases, and among them, at least 2% are sure to have suboptimal sperm parameters. Sperm analysis tests help check the sperm parameters, such as sperm morphology, sperm count, and sperm motility.
Every couple having fertility issues goes through a complete checkup, blood analysis, hormone testing, imaging scans, and sperm analysis to understand the exact reason for infertility. Of them, semen analysis is an important fertility test prescribed to check sperm quality and quantity.
In countries like India, where testing for male fertility factors is still a denied act or unacceptable, men who take the test may experience anxiety and nervousness about these tests.
This article dives into what you can expect during a semen analysis and analysing a normal and abnormal semen analysis test report.
Also Read: https://pregajunction.com/blog/semen-analysis-test-price-in-india/
In this Article
Get a consultation with the best specialist in your Location
Get a consultation with the best specialist in your Location
Semen Analysis test: What is it?
Semen analysis, referred to as the sperm count test, analyzes the quantity and viability of the semen sample. Semen, a fluid ejaculated from a man’s genitals contains sperms that fertilise with a woman’s egg when released into the female reproductive tract. The health and potential of the sperm to fertilise with the egg decide the sperm factors of male fertility.
A semen analysis test measures sperm factors, such as:
- Sperm Numbers or sperm count,
- Sperm shape or sperm morphology,
- Sperm movement or sperm motility.
Sperm count changes every day, and an average of two to three sperm analysis tests conducted in a span of seven days or within two to three months can give the doctors a fair idea of the sperm condition and conclusive results.
Reason to take the sperm analysis test
Your fertility specialist may suggest a sperm analysis test to examine the below conditions.
- Problems in getting pregnant
- Reasons for sperm dysfunction and ejaculation issues
- Analyse the success of vasectomy, surgery performed in men for birth control.
How is a semen analysis test performed?
It is essential to follow guidelines before taking the semen analysis test. Some of the prerequisites of a semen analysis test include:
- Do not ejaculate for at least 24 to 72 hours before the test.
- Stay away from alcohol, caffeine, and drugs for five to seven days before the test.
- Certain herbal medications can affect hormones and sperm production. Avoid herbal medications or check with your specialist about the same.
- Inform your specialists about the hormone medications and other medicines you are taking and know whether to avoid them or not before the test.
The semen sample is collected in a sterile container mainly by self-stimulation or masturbation. Otherwise, artificial extraction methods are also considered.
If the semen sample is collected at home, it is necessary to deliver the sample within a timeframe as the sperm needs to be evaluated within two hours of ejaculation. One can also opt for the clinic’s separate sperm collection room to take the semen sample.
A normal and abnormal semen analysis report
The normal range values differ between clinics and laboratories. However, the normal minimum values demarcated by the World Health Organisation (W.H.O) are mentioned below.
| Sperm Parameters | Lower Reference range |
| Semen volume | Between 2 millilitres (mL) to 5 ml of fluid |
| Total sperm count | 40 million to 300 million sperms per mL of fluid |
| Sperm concentration | A minimum of 15 million sperms per mL (million/mL) of semen |
| Total motility | 40-50% of motile sperms with movement quality of 2 or higher on a scale of 0 to 4. |
| Progressive motility | 31 to 34 % |
| Vitality or viability | 50% of the sperm cells should be viable |
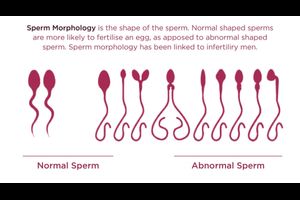
| Sperm morphology | Normal shaped cell will have a distinct head, midsection, and tail with proper measurements and proportions between each. 4 % of the sperms must have normal shape. |
| Liquefaction | Semen should liquefy within 20 minutes of ejaculation. |
| Semen pH | Should range between 7.2 to 7.8 |
| Semen WBC count | The semen WBC count should be less than 1,000,000 per mL of semen |
The WHO has definite lower reference limits for semen characteristics. Having more or less than the given set of sperm parameters does not necessarily signify infertility. Your doctor will study the test report based on the set guidelines.
Below is a list of what each sperm parameter refers to and its abnormal indicatives.
| Sperm parameter | Abnormal range | Possible indications |
| Semen volumeRefers to the total ejaculate volume of the semen | Lower than 2- 5 ml of semen |
|
| Total sperm count
Total sperm count is the total number of sperm present in one ejaculate |
Lower than 39 million sperms per mL of ejaculate |
|
| Sperm Concentration
Number of sperm found in one mL of semen |
Less than 15 million sperms per mL of semen |
|
| Sperm motilityPercentage of motile sperms or moving sperms | Less than 40% of motile sperms and movement quality less than 2 on a scale of 0 to 4. |
|
| Sperm viability or vitalityPercentage of live sperms in the semen sample. | Less than 50% of viable sperms |
|
| Sperm morphologyShape and size of the sperm cells | Less than 4% of normal shaped sperm cells |
|
| Semen liquefactionTime taken by the semen to liquify allowing the sperms to swim better | Delayed liquefaction time- more than 20 minutes |
|
| Semen pHMeasurement of acidity or alkalinity of the semen | More than 8.0 or less than 7.0 |
|
| Semen WBC countThe WBCs present in the semen sample that help fight infections | Higher than 1,000,000 per mL of semen |
|
In case of abnormal or irregularities in the semen analysis report, your fertility specialist may suggest another semen analysis after a few weeks. Repeated abnormal semen analysis reports may require additional tests to examine the underlying fertility condition. And accordingly, lifestyle modifications or treatment processes can be decided.
What if the reports are abnormal?
An abnormal semen analysis outcome need not necessarily indicate a sign of impaired fertility. The abnormal sperm factors may be due to stress, hormonal changes, anxiety, illness, infection, certain medications, lifestyle, and environmental factors.
The specialists decide the line of treatment depending on the sperm fertility factors and the exact reason for infertility. Here are some of the options your fertility specialist is likely to consider.
Hormone treatments: Imbalances of hormones and fluctuating hormones causing low sperm numbers can be treated through hormonal therapies and medications.
Surgery: Surgeries can help correct varicocele and reverse vasectomy to help improve sperm counts.
Treating infections and medical conditions: Treatment of infections and medical conditions such as celiac disease and thyroid imbalance can help improve fertility chances.
Testicular sperm extraction. In cases of low sperm count, no sperm, or ejaculation, microsurgical sperm extraction is an option. The sperms are extracted directly from the sperm-producing testicles through a needle and used in infertility treatment procedures like IUI, IVF, or ICSI.
Intrauterine insemination (IUI): IUI treatment involves semen sample extraction and processing. The washed and processed semen is inseminated through the cervix into the woman’s uterus.
IVF or IVF-ICSI: IVF treatment requires retrieval of sperm and egg that are fertilised in incubated laboratory conditions, and the fertilised egg is transferred into the woman’s uterus. . In IVF with ICSI, a single viable selected sperm is directly injected into an egg. Major sperm fertility factors are taken care of through IVF and ICSI fertility treatment procedures.
Lifestyle changes: Healthy diet and habits such as quitting smoking, alcohol consumption, and drugs must be eliminated to improve sperm counts.
Sperm donor options: Certain sperm fertility conditions may require couples to consider sperm donor options.
Also read: https://pregajunction.com/blog/semen-analysis-report-how-to-read-a-sperm-analysis-test-report/
Get a consultation from the best IVF center of your Location
Get a consultation from the best IVF center of your Location
Frequently Asked Questions
1-What is the normal sperm count to get pregnant?
Sperm count is the number of sperms present in the provided semen sample. To get pregnant, at least 20 million per millilitre (m/mL) sperm per ejaculate is sufficient. However, the normal sperm count range considered is 40 million to 300 million sperm per mL of ejaculate.
2-What is an abnormal sperm report?
The semen analysis test report is abnormal when a man’s sperm parameters fall below the normal ranges of minimum sperm characteristic requirements. The doctor may advise further tests or a repetitive sperm analysis to understand the condition and cause of abnormal sperm factors.
3-How do I read my sperm analysis report?
The major parameters present in a semen analysis test report are:
- Semen ejaculate volume: lower than 2-5 ml of semen ejaculate volume indicate failed emission, improper ejaculation, blockage, or absence of ducts.
- Sperm concentration: lesser than 15 million sperms per mL of semen means low sperm count or oligospermia. Lower than 5 million sperms/mL of semen means a severely low sperm count.
- Sperm motility: 50% and above motile sperms gives better chances of fertility and pregnancy. Less than 50%- poor motile sperms or asthenozoospermia.
- Sperm morphology: Less than 4% of normal-shaped sperms indicate abnormally shaped sperms or teratozoospermia.
Conclusion
Semen analysis test calls for careful semen sample collection and analysis of multiple sperm characteristics. The test report provides various sperm information that can help determine the sperm factors affecting fertility in a man.
In case of abnormal test results, your fertility specialist may conduct another semen analysis after a few weeks or further proceed with additional tests to understand the underlying male infertility cause.