Pregnancy is a time of many changes in a woman’s body and mind. However, there is a high chance of every pregnancy having some risks or problems. Sometimes things go wrong during pregnancy and you need extra care. One can have problems either because of a health condition they had before getting pregnant or because some complications develop during pregnancy. Even issues with previous pregnancy (if any), drug & alcohol use during pregnancy, being pregnant with twins or more, or being over age 35 – can be some other most common reasons which cause problems during pregnancy. Any of these complications can affect the health of both – your health and your baby.
Sometimes, the most significant part of your body which supports a pregnancy – the umbilical cord and the placenta, can develop abnormalities and stop functioning normally and create problems.
In this article, we are going to discuss common complications with Umbilical cord and Placenta.
In this Article
What is the umbilical cord?
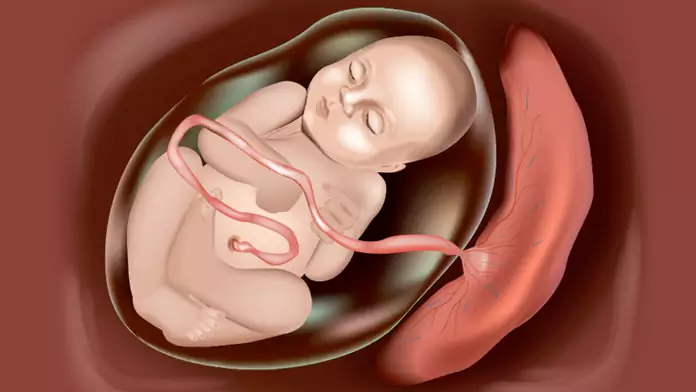
During pregnancy, the umbilical cord is the lifeline joining you and your baby. The umbilical cord is a flexible, tube-like structure that has a spongy appearance. A jelly-like substance that surrounds and protects the cord. The umbilical cord connects your baby to your placenta and contains two arteries and one vein. Oxygen and nutrient-rich blood are provided to your baby and it also carries the baby’s waste products.
The baby doesn’t need the umbilical cord any longer once they are born. The umbilical cord is cut, shortly after birth, leaving a short piece of it called a stump, attached to your baby’s belly button. The stump dries up naturally and usually falls off within a few weeks after birth. Don’t pull the cord off on your own. Make sure the cord is dry and clean to prevent infections.
Structure of the Umbilical Cord
Your baby’s umbilical cord connects from the navel to the placenta and is usually a three-vessel cord.
Your baby’s umbilical cord has three layers:
- Tunica externa – this outermost protective layer is made of a thick elastic-like fiber.
- Tunica media – this layer contains most of the umbilical cord’s blood vessels. It helps to regulate your baby’s blood flow and blood pressure.
- Tunica interna – this connective tissue has valves controlling blood flow. It allows for the deoxygenated blood to be moved to the placenta and oxygenated blood moved back to your baby.
Problems with Umbilical Cord
Let’s learn more about these abnormalities and find out when you should be concerned.
- Single Umbilical Artery – Normally your baby should have an umbilical cord with two arteries and one vein which is known as a three-vessel cord. Sometimes one of the arteries is missing, usually the left one and there are only two vessels —usually one vein and one artery.
If the umbilical cord only has one artery (called a two-vessel cord), it poses a greater risk for fetal abnormalities. Single artery umbilical cord problems only happen in around 1% of pregnancies, however, it increases to 5% in the case of twin pregnancies.
Associated Risks – A two-vessel cord increases the risk of:
- Your baby being smaller than average
- You having high blood pressure toward the end of your pregnancy
- Infantile death soon after birth
- Trisomy 18
- Cardiovascular anomalies
- Gastrointestinal problems
- Esophageal atresia
- Kidney issues
Causes – Causes of this complication are largely unknown. However, if you have diabetes, you’re more likely to have a single artery umbilical cord.
Diagnosing a single umbilical artery – It is easily identified on ultrasounds during your pregnancy. Usually, the vein is larger and distinguishable from the two arteries. Only a single artery may be noted after looking at a cross-section of your umbilical cord. A perinatologist, an obstetrician who specializes in high-risk pregnancies, will likely be recommended to you by your doctor.
- Vasa Previa – Vasa previa is a condition that occurs when the fetal vessels attach near the cervix. Due to the possibility of the cord rupturing when your water breaks during birth, this condition is risky. It could happen close to the membrane separating twins from one another in the womb.
Risks of vasa previa – This condition doesn’t pose any risks during pregnancy itself. However, if the vessels tear during labor, there is a 50-75% chance of infant death during delivery. Even if vessels don’t tear, the pressure of labor might reduce oxygen while delivery and put the baby in distress.
Causes of vasa previa – The cause is unknown, although it is associated with a low-lying placenta and if you’re carrying twins or more.
Diagnosing vasa previa. This condition is often identified using ultrasound imaging during your pregnancy. If it isn’t identified on an ultrasound, it may become evident during labor if your baby’s heart rate drops. If undiagnosed, vasa previa, the doctor may recommend a cesarean delivery between 34-37 weeks.
- Nuchal Cord – A nuchal cord occurs when the umbilical cord wraps around the fetal neck completely or for 360 degrees. The term “nuchal” relates to the nape or back of the neck.
Risks of nuchal cord – Most of the time, this condition won’t cause any problems. In rare cases, labor induction may be required to ensure a prompt delivery. A nuchal cord increases the risk of a longer labor for you and a decreased heart rate of your baby during contractions.
Causes of nuchal cord – The cord easily wraps around different parts of the baby’s body when they move around in the womb. In fact, the cord may wrap and unwrap multiple times throughout your pregnancy as your baby stretches and grows.
Diagnosing a nuchal cord. As with other umbilical cord abnormalities, an ultrasound frequently diagnoses the condition. If undiagnosed before labor, it may become apparent if your baby’s heart rate decreases consistently with each contraction.
- Umbilical Cord Knots – An umbilical cord knot happens when your baby moves around in a manner that causes a loop in the cord as if it were tied.
Risks of a cord knot – Usually, an umbilical cord knot doesn’t get tight enough to cause harm. However, a true knot may cut off blood flow to your baby, increasing the risk of them losing oxygen and nutrients. This may lead to brain damage and even stillbirth. A cord knot may lead to cesarean delivery for a birth free of complications.
Causes of an umbilical knot – Identical twins sharing a single amniotic sac, too little amniotic fluid, a longer umbilical cord or a smaller baby that has more room to move are some factors that increase the likelihood of an umbilical cord knot.
Diagnosing an Umbilical Knot – Most of the time, a knot doesn’t show up on ultrasound imaging. Because the cord is long, parts of it may be covered when a technician is checking your baby.
Problems with Placenta
Now that we have extensively covered the umbilical cord, let’s shift our focus to learning about the placenta and its possible complications during pregnancy.
What is the placenta?
The placenta is an organ that develops in the uterus during pregnancy. It provides oxygen and nutrients to your baby. It also removes waste products from the baby’s blood. The placenta attaches to the wall of the uterus, and the baby’s umbilical cord arises from it. It’s attached to the top, side, front or back of the uterus.
Factors affecting placental health
During pregnancy, different factors can affect the placental health. Some of them are:
- Mother’s age – After age 40, some problems with the placenta are more common.
- Leaking Amniotic Fluid – The risk of certain problems with the placenta increases if the amniotic sac leaks or breaks before labor begins.
- Twin or other multiple pregnancies – Carrying twins also might increase the risk of certain problems with the placenta.
- High blood pressure. High blood pressure can affect the placenta.
- Previous uterine surgery – A C-section or surgery to remove fibroids, increases the risk of certain problems with the placenta.
- Substance use. Some placental problems are more common in women who smoke or use drugs during pregnancy.
- Abdominal trauma. Trauma to your abdomen (such as from a fall, auto accident, etc), increases the risk of the placenta prematurely separating from the uterus (placenta abruption).
Here’s what you need to know about the possible placental problems during pregnancy:
- Placenta Previa – Placenta previa is when a pregnant woman’s placenta partially or completely blocks the opening to the cervix – the opening of the uterus. During a vaginal delivery, your baby passes into the cervix and through the birth canal. Normally, the placenta attaches toward the top of the uterus, away from the cervix.
What happens with placenta previa is that, as the cervix opens during labor, it can cause the connecting blood vessels (from the placenta to the uterus) to tear. This can lead to bleeding and put both the baby and mother at risk.
Types of placenta previa
Marginal previa, also called the low-lying placenta, is when the placenta is close to the opening of the cervix but doesn’t cover it.
Complete previa is when the placenta covers the entire opening of the cervix.
Risks involved with placenta previa – Placenta previa can cause severe vaginal bleeding during pregnancy or delivery. If placenta previa persists late in the third trimester, a C-section will be recommended.
Causes of placenta previa – Some of the possible causes and risk factors of placenta previa include:
- Low implantation of the fertilized egg
- Abnormalities of the uterine lining, such as fibroids
- Abnormalities of the placenta
- Multiple babies, such as twins
- Multiple pregnancies – a woman who has already had six or more deliveries has a risk of one in 20.
Diagnosing a Placenta Previa – Placenta previa is often diagnosed during an ultrasound on your routine prenatal visits. The test uses sound waves to show if the placenta covers the opening from the womb to your cervix.
Apart from Placenta previa, some other placental problems may include –
- Placental Abruption – which happens when the placenta peels away from the inner wall of the uterus before delivery either partially or completely. This can deprive the baby of oxygen and nutrients and cause heavy bleeding. Placenta abruption may result in an emergency situation that requires an early delivery.
- Placenta accreta – Generally, the placenta detaches from the uterine wall after childbirth. However, in the placenta accreta, part or all of the placenta remains firmly attached to the uterus. It can occur when the placenta’s blood vessels and its other components grow too deeply into the uterine wall. It can cause severe blood loss during delivery.
In some critical cases, the placenta invades the muscles of the uterus and the doctors mostly recommend a C-section followed by uterus removal. - Retained placenta – If the placenta doesn’t deliver within 30 minutes after delivery, it’s known as a retained placenta. It might occur if the placenta gets trapped behind a partially closed cervix or because the placenta is still attached to the uterine wall. A retained placenta can cause severe infection or life-threatening blood loss if left untreated.
FAQs
-
How do I know if my baby’s umbilical cord stump is not healing properly?
It’s typical to see a little blood near the stump during the healing process. However, if the umbilical area oozes pus, the surrounding skin becomes red and swollen, or the area develops a pink moist bump you must contact your baby’s healthcare provider. These could be signs of an umbilical cord infection. Timely treatment is needed to stop the infection from spreading.
-
What are common signs or symptoms of placental problems?
The most common symptoms of placental problems include – Vaginal bleeding, abdominal pain, back pain and uterine contractions. Consult your doctor/ health care provider during pregnancy if you have any of these symptoms.
-
How can I reduce my risk of placental problems?
Most placental problems can’t be prevented however steps must be taken to promote a healthy pregnancy. Regular prenatal visits, and managing health conditions such as blood pressure, no smoking, etc can reduce your risk of potential placental problems.
Conclusion
Problems with your baby’s umbilical cord and the placenta can affect the health of both you and your baby. Both these issues can lead to an emergency situation if not treated correctly and in a prompt manner. However, being better informed can significantly reduce your risk of having a difficult delivery. Now that you are well informed about the umbilical cord and the placenta, hopefully, you are better equipped to handle it, should the situation arise. Make regular prenatal visits and make appointments with your doctor if you have any of the signs or symptoms mentioned above. If it’s severe, go to the hospital. If you still have questions about the umbilical cord or placental problems, you can talk to your doctor.