Since the inception of Assisted Reproductive Technology (ART), procedures have become more refined and evolved throughout the years. The field of embryology has experienced exponential growth, followed by higher rates of successful pregnancy outcomes. In-vitro fertilization (IVF), which started in the 1970s, yields over 2.5 million cycles globally.
Every patient undergoing IVF expects successful results to enjoy the ride of parenthood. New technologies are constantly developed, primarily to support the treatment. Besides the basic IVF procedures, several add-on technologies are gaining traction for ensuring better chances of the cycle’s success.
The list of IVF add-on procedures is quite long. However, a handful of evolved treatments have secured a place for themselves in the market. We will be exploring the top add-ons that are primarily practiced worldwide as part of the ART procedures.
Also Read: COVID 19 Vaccination Doesn’t Affect IVF Success Rates, New Research Study Claims
In this Article
- 1 IVF Add-Ons – Everything you Need to Know
- 1.1 1. Time-Lapse Imaging of Embryos
- 1.2 2. Assisted Hatching (AH)
- 1.3 3. Hyaluronan‑enriched Media (EmbryoGlue)
- 1.4 4. Sperm DNA Fragmentation Testing
- 1.5 5. Artificial Oocyte Activation (AOA)—Calcium Ionophore
- 1.6 6. Endometrial Receptivity Arrays (ERA)
- 1.7 7. Physiological Intracytoplasmic Sperm Injection (PICSI)
- 2 Conclusion
IVF Add-Ons – Everything you Need to Know
The IVF add-on interventions make up a long list of gradually evolving procedures. Some are practiced commonly around the world, while a few others are still in the primary stages of testing. This article will explore the top 7 procedures, their definition, and their significance in detail:
- Time-Lapse Imaging of Embryos
- Assisted Hatching
- Embryoglue
- Sperm DNA Testing
- Egg Activation with Calcium Ionophore
- Endometrial Receptivity Array
- Physiological Intracytoplasmic Sperm Injection (PICSI)
Besides the current face and use of these technologies, we will also explore their future directions and implications in the long run.
1. Time-Lapse Imaging of Embryos
When it comes to IVF procedure, the first step towards success is to fertilize the egg and the sperm to form the embryo eventually. Most of the cycles fail due to a lack of vigilance during this first step.
With the Time-Lapse Imaging of Embryos, the embryologists use digital cameras to consistently monitor the growth and development of the fertilized embryo in the culture media. The cameras are built into an incubator to prevent alternations in the culture media and its environment.
The tool finally came into being in 2014, following a randomized controlled trial that evaluated the overall technology and its efficacy in the field of IVF and assisted reproduction. The primary significance of the TLI technology was that it recorded even the minute changes and developments in the embryo, which otherwise wouldn’t be known.
The researchers are still looking into the actual clinical benefit of this procedure. Contrary to popular belief, TLI doesn’t increase any obstetric or perinatal adverse risks.
Significance of TLI:
- It improves the overall success rates of the treatment
- It keeps a close eye on the development of the embryo through each stage
- It improves the predictive accuracy for selecting the optimal embryo for the uterine implant
Risks or Downsides of TLI:
It is with no doubt that TLI improves the prospective outcome of the IVF success treatment. However, implementing this technology into the clinical setting is extremely expensive. In a report, around 50% of embryologists refused to use TLI due to the expense it came with. Another 37.5% reported a lack of data supporting the overall clinical value of this technology.
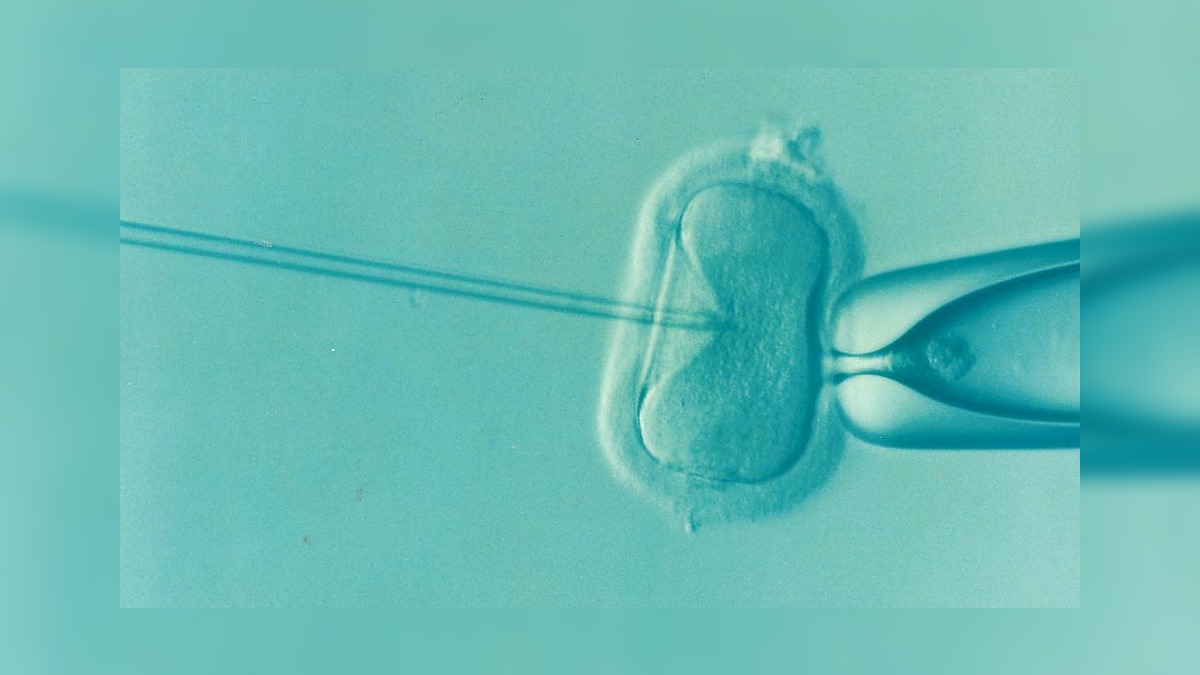
2. Assisted Hatching (AH)
The advent of Assisted Hatching goes back to 1988, which means the procedure isn’t fairly new. Later in 2006, a randomized study found better impacts of the AH in improving implantation and pregnancy rates in patients undergoing IVF. The same didn’t have much difference in patients undergoing fresh embryo transfer.
Assisted Hatching uses a laser to create a small hole into the zona pellucida to promote the embryo to “crack” from its shell. The procedure has potent benefits in individuals with a poor prognosis surrounding the pregnancy or previous unsuccessful IVF cycles. Although the procedure is used in mainstream ART procedures, it still lacks clinical evidence.
Significance of AH:
- It improves the chances of a successful IVF treatment in patients with failed IVF cycles
- It is effective for patients who experience issues with successful embryo implant
Risks or Downsides of TLI:
More than the benefits, the lack of clinical evidence and potent risks make AH a very non-conducive procedure more than the benefits. The most significant risk with AH is that it enhances the chances of conception of multiple babies, leading to further pregnancy complications in the patients. Also, poking at the zona pellucida often results in chromosomal changes or congenital fetal anomalies. It can also lead to fetal malformations.
3. Hyaluronan‑enriched Media (EmbryoGlue)
With IVF or any form of ART procedure, the biggest worry lies during the implantation process. Many factors contribute to this issue, primarily due to the embryo “not sticking” to the uterine lining.
The use of EmbryoGlue or an enriching transfer media with Hyaluronan has been found to enhance those chances of successful implantation. The procedure was initially introduced in the 1990s, following which its importance has stood out as an add-on IVF procedure.
Following this, further studies suggest that a higher concentration of hyaluronan in the culture media mimics the uterine fluid and improves the rates of decidualization of the uterine lining. The clinical use of EmbryoGlue started in 2003. The efficacy of using hyaluronic acid in the transfer media proved to have better impacts on live births and successful pregnancies from the IVF procedures, as recorded in a recently 2020 study.
Due to its effectiveness and minimal risks, EmbryoGlue currently has an amber rating under HFEA. However, this also indicates that more laboratory and clinical trials are needed to chalk the benefits of this add-on procedure better.
Significance of EmbryoGlue:
- It improves the embryo’s implantation rate
- It mimics the intrauterine environment in the transfer media for better success rates
- It is a cost-effective procedure
Risks or Downsides of EmbryoGlue:
The use of EmbryoGlue during IVF procedures has little to no risks on the embryo and the patient. However, reports do suggest that it enhances the chances of conceiving multiple babies during the cycle.
4. Sperm DNA Fragmentation Testing
Optimal sperm health is a key contributor to the successful conception via an IVF procedure. However, previous studies indicate that DNA breaks or DNA fragmentation contribute to poor sperm quality and can eventually lead to infertility in male patients.
Currently, there are four types of Sperm DNA fragmentation testing available. They include:
- Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL)
- Sperm Chromatin Structure Assay (SCSA)
- Sperm Chromatin Dispersion (SCD)
- Comet Assay
These tests assess sperm quality and sperm function that contribute to the overall success of a natural conception or assisted reproductive technology. The techniques and testing were initially introduced in the 1980s but started as pre-clinical trials on animals.
The prevalence of DNA fragmentation in the sperm cells reduced the chances of successful conception after IVF cycles. The European Association of Urology recommends Sperm DNA fragmentation testing in couples with multiple recurrent pregnancy losses (either through natural conception or IVF).
Significance of Sperm DNA Fragmentation Testing:
- It gives complete profiling of the sperm quality and sperm functions
- It allows the patients to find a reason behind their infertility to take the right steps for conception in the future
Risks or Downsides to Sperm DNA Fragmentation Testing:
The Sperm DNA Fragmentation Testing doesn’t impose any notable risks to the male patients undergoing the procedure. The sperm is collected from the patient’s semen sample. The procedure becomes invasive if the male patient undergoes testicular sperm extraction (TESE) procedure for testing the degree or presence of DNA fragmentation in the patients. Not to mention that the procedure is comparatively expensive too, ranging between USD 170-250.
5. Artificial Oocyte Activation (AOA)—Calcium Ionophore
Calcium Ionophore is a potent chemical that promotes oocyte activation and thereby fertilization. The basis of this add-on technology again dates back to the 1970s that initially started with animal studies. Following the effectiveness, clinical trials began, which proved similar results.
However, the use of AOA has potent benefits in fertilization but lacks enough data to find its efficacy on pregnancy and overall live birth rates. Even studies suggest no significant changes following the use of AOA in infertile couples. Although AOA doesn’t necessarily directly impact the pregnancy rates and successful chances of conception, it improves the overall parameters that support the pregnancy journey.
Significance of AOA:
- It improves the chances of fertilization during IVF procedures
- It improves fertilization, blastocyst, implantation rates, and live birth rates
- It improves the chances of conception in patients undergoing ICSI procedure
Risks or Downsides to AOA:
Although the benefits to AOA are quite profound and globally acknowledged, there are controversies surrounding the safety of this procedure. One of the biggest risks was the increased chances of birth defects in the fetus. Studies also found that AOA leads to risks of preterm delivery or intrauterine growth restriction during pregnancy. It also contributes to adverse neonatal outcomes in the patients.
6. Endometrial Receptivity Arrays (ERA)
Another popular add-on procedure suggested with IVF is ERA or Endometrial receptivity arrays. Since the endometrial environment and receptivity play a crucial role in the successful implantation of the embryo, checking these parameters is crucial.
The ERA is a procedure that assesses the molecular make-up of the endometrium. In simpler words, it allows the specialists to check the condition of the endometrium and check for existing anomalies. The procedure helps identify the ideal window time of implantation for heightened success rates of the pregnancy. The procedure was initially introduced in 2011.
Significance of ERA:
- It helps specialists identify the optimal window for embryo implantation in the endometrium
- It analyzes the sensitivity of the endometrium and pinpoints risks and anomalies too
Risks or Downsides to ERA:
ERA is quite a simple procedure with fairly minimal risk. However, the procedure isn’t non-invasive. The tissue collection mimics the procedure of endometrial biopsy, which can be painful for the patient. The same can even lead to heightened risks of intrauterine injury or infection. That aside, ERA is an extremely expensive procedure, ranging between USD 800-1000.
7. Physiological Intracytoplasmic Sperm Injection (PICSI)
Last on the list of IVF add-on techniques is PICSI or Physiological intracytoplasmic sperm injection. With IVF procedures, selecting the highest grade of the sperm and egg is crucial for successful fertilization and conception in the patient. With PICSI, the specialists identify the sperm that binds the best with the Hyaluronic Acid (HA) in the transfer media. This enables the selection of the sperm with optimum genomic activity and reduces the risks of aneuploidy and miscarriages in the patients.
The introduction of PICSI dates back to the early 2000s and was later better recognized in 2010, following a study that found that using PICSI improved embryo quality in the IVF journey.
PICSI is a highly sensible add-on procedure with IVF, especially potent in patients who have experienced previously failed IVF cycles. The procedure doesn’t affect the live birth rates as well. There is a low quality of evidence but studies indicate that using PICSI reduces the miscarriage levels subsequently well.
Significance of PICSI:
- It helps with the selection of the most potent sperm with optimal genomic integrity
- It ensures higher IVF cycle success with healthy fertilization and implantation
- It reduces risks of aneuploidy and miscarriages
- It doesn’t affect the live birth rates
Risks or Downsides to PICSI:
The primary downside to PICSI is its lack of impact on pregnancy outcomes. This is why most patients don’t find it lucrative to spend an additional amount on a procedure that won’t make a drastic difference in the long run, especially about the success rates of the procedure. Specialists suggest that PICSI should only be offered to the patients in research settings instead of clinical practice.
Conclusion
The availability of IVF add-ons is quite long. The list of procedures mentioned in the article are more “known” and used procedures. However, many other options are undergoing clinical trials and are in the beginning stages of research.
The future of these add-on procedures is still uncertain. Specialists believe that the only add-on procedures that provide true efficacy and make a difference in the pregnancy outcomes in the future of IVF will stay. Some of these existing add-ons are also undergoing refining and perfecting to make them an integral part of the clinical practice.