Over the last three decades, infertility treatments have not just evolved but become more refined, promising higher success rates. Assisted reproductive techniques (ARTs) like Intracytoplasmic sperm injection (ICSI) are often done in conjunction with in-vitro fertilization (IVF) to ensure a successful conception for couples.
Unlike IVF, which is solely for female factor infertility, ICSI is often a chosen route to bridge the issues with male factor infertility. Before developing IVF/ICSI techniques, the process of ART was very limiting. Thankfully, things have progressed for the better now.
This article will explore the meaning of intracytoplasmic sperm injection, its ideal candidates, success rates, and associated costs.
In this Article
What is Intracytoplasmic Sperm Injection (ICSI)?
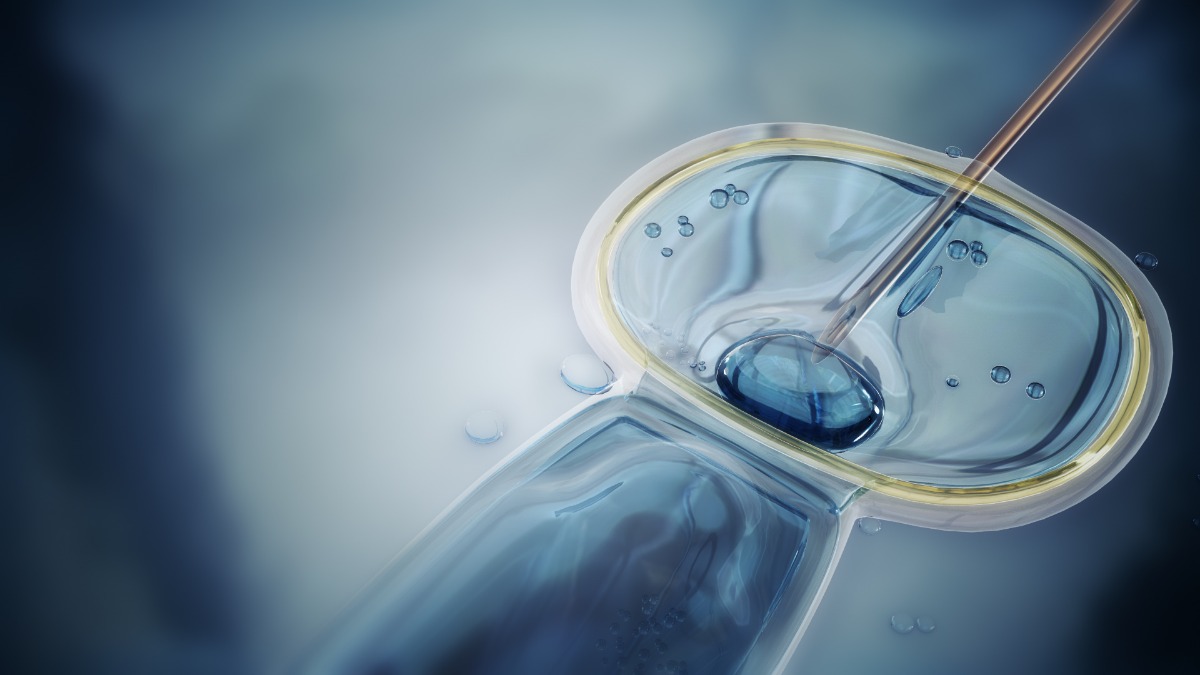
ICSI is a subset of IVF in which a washed and treated sperm from the collected semen sample of the male patient (or donor) is injected directly into the cytoplasm of the egg of the female patient. This reduces the risks of acrosome reaction and assures a successful fusion of the gametes to produce an embryo.
Unlike a standard IVF procedure where 40,000 – 50,000 sperm cells are used for successful fertilization, in ICSI, the most potent sperm cell is directly fused into the female gamete.
Following the successful fertilization of the male and the female gametes, the developed proembryo is then transferred to the uterus for successful implantation and conception.
ICSI helps combat male factor infertility. This is done and advised for male patients with an abnormal semen analysis test and impotent sperm function (and motility).
Who are the Ideal Candidates for ICSI?
If you are consulting a fertility specialist after trying to get pregnant, the chances are that they will first suggest undergoing a host of physical and pathological testing. If the male partner has abnormal test results from these tests, only then would your doctor suggest a combined treatment with IVF and ICSI for a successful conception.
You will need to opt for ICSI if:
- Have low sperm count
- Have low sperm motility
- Have poor sperm morphology
- Had lesser success with previous IVF treatments
- Require surgical sperm retrieval
- Using frozen sperm due to age factors
These are some of the most common and prominent reasons your fertility specialist might consider ICSI. Suppose the issue with infertility in a couple is prominently due to male factors. In that case, the chances are that an ICSI is the only chance at a successful conception and healthy pregnancy for the couple.
What can I expect while Undergoing ICSI?
ICSI is an extensive process. It isn’t a decision that’s taken and implemented in a day. It involves a lot of discussion with the doctor, a proper understanding of what to expect, and a conclusion.
Since the procedure is in conjunction with IVF, both the female and the male partner must undergo simultaneous procedures to ensure a successful conception.
In traditional IVF, over 50,000 swimming sperm from the semen sample is placed in a laboratory petri dish with the retrieved egg. It is left in optimal condition for that one sperm cell to fertilize the egg and form an embryo. The failure of this step is why ICSI is done.
With ICSI, the embryologist will isolate the healthiest sperm cell from the collected sample and directly inject it into the egg’s cytoplasm to promote fertilization.
Ideally, the process is done in three stages:
- Sperm collection
- Ovulation and egg retrieval
- Sperm injection and transfer
Let us elaborate on each of them for you:
Sperm collection
The main part of the ICSI procedure is to collect the most potent sperm cell that can help with the fertilization process. If the male patient fails to perform, the doctors can retrieve the sperm sample from the testicle with a minimally invasive procedure. The procedure is commonly done in patients with diagnosed blockage in their reproductive anatomy.
Once the semen sample is collected, the sperm cells are isolated, washed, and treated. The cells also undergo screening for genetic anomalies before using them in the ICSI procedure.
Ovulation and egg retrieval
As we said, not just the male partner, even the female partner undergoes a simultaneous procedure for ICSI. The patient undergoes follicle-stimulating hormone shots at least two weeks before the egg retrieval procedure. During the second week, the doctor will run salient testing and imaging to check the ovulation status and see if the follicles have fully matured or not.
If yes, a shot of human chorionic gonadotropin (hCG) is given to stimulate ovulation, and the matured eggs are retrieved around 34-36 hours later. The egg retrieval procedure is done via a laparoscopic procedure.
Sperm injection and transfer
The last and the most crucial part of the ICSI is the sperm injection. In this stage, the retrieved egg is placed on a petri dish and held with a tiny glass tube. On the other hand, a micropipette is used to inject the treated sperm cell directly into the egg’s cytoplasm. The culture is left overnight under optimal conditions and monitored to check for fertilization.
After 3-5 days of incubation, the successfully fertilized eggs are taken. Amidst them, one or more are placed into the uterus for successful implantation and pregnancy.
IVF-ICSI is an extremely taxing process, both physically and emotionally. The series of shots, hormones, and injections can take a toll on the patient’s body. However, the lingering series of “what ifs” can also crowd the patients’ minds. Despite all of these changes, the procedure has a pretty high success rate and brings happiness to people.
What is the Success Rate of ICSI?
A successful ICSI procedure will fertilize 50-80% of the eggs. Although this might not seem like much to begin with, it is a lot compared to the 0% that initially had the lingering male factors.
Studies have found that ICSI produces around 25-30% birth rate after a successful conception with the IVF procedure.
However, it is always ideal to have a transparent understanding of the situations. Although ICSI enhances the chances of a successful conception, it comes with a few complications too. Some of them include:
- The procedure can damage all the retrieved eggs from the female patient
- The fertilized egg might not grow or develop into an embryo
- The embryo may seize growing suddenly, leading to no implantation or eventual miscarriage
Also, pregnancy with IVF-ICSI often leads to multiple pregnancies, often treated as a risk or consequence in medical terms.
How much does ICSI Cost?
The cost of the Intracytoplasmic Sperm injection procedure will vary from country to country. Not just the place, even the doctor’s expertise, the allied charges, etc., will make the treatment costs subjective.
In the United States and western countries, the rates for ICSI range from $800 to $2500 per cycle. The cost can range from INR 2,40,000 to INR 2,80,000 per cycle in India.
FAQs
Conclusion
ICSI or Intracytoplasmic Sperm injection procedure is gaining gradual prominence in the medical field. Thanks to its growing success rate, more and more male patients are becoming comfortable seeking the help they need to form a biological family with their partner. However, since the procedure does come with its set of risk factors, ensure that you consult the best in the field for refined and desired results.